Considerations To Get Your CAR T Testing Strategy Right
By David Colter, Ph.D., Sr. Director of Analytical Development, Center for Breakthrough Medicines
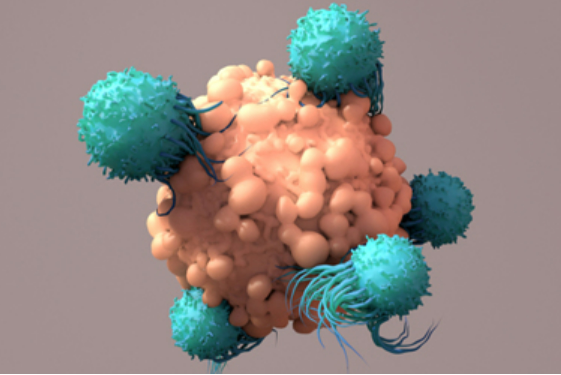
Less than five years after the first approval of a CAR T therapy in 2017, momentum for CAR T and other cell therapies has never been greater.
Given their experience reviewing and approving six CAR Ts across 10+ indications, the FDA released a draft guidance “Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products” in March of 2022. As a trusted partner to cell therapy product developers such as Achilles Therapeutics, we at the Center for Breakthrough Medicines (CBM) identified three considerations – testing CAR-T starting material, establishing manufacturing process controls, and implementing robust testing analytics – that our clients prepare for as part of their analytical development prior to finalization of the guidance. This will help to monitor and report on the right critical quality attributes (CQAs) of their CAR T products which is needed for characterization of the product’s safety and efficacy that is reported to health authorities.
What CAR T Innovators should take away from the FDA’s March 2022 Draft Guidance
Less than five years after the first approval of a CAR T therapy in 2017, momentum for CAR T and other cell therapies has never been greater. In the last two years, two additional CAR T therapies (Abecma, Carvykti) were approved newly targeting the BCMA antigen. Prior approvals targeting CD19 include Breyanzi, Kymriah, Tecartus, and Yescarta (which was also granted an expansion into 2nd line treatment in spring of 2022). Looking forward, regulatory decisions are expected for other cell therapy including Iovance’s Lifileucel Tumor-Infiltrating Lymphocytes) and Gamida Cell’s Omidubicel (allogeneic hematopoietic stem cell).
Given their experience reviewing and approving six CAR Ts across 10+ indications, the FDA released a draft guidance “Considerations for the Development of Chimeric Antigen Receptor (CAR) T Cell Products” in March of 2022. As a trusted partner to cell therapy product developers such as Achilles Therapeutics, we at the Center for Breakthrough Medicines (CBM) identified three considerations – testing CAR-T starting material, establishing manufacturing process controls, and implementing robust testing analytics – that our clients prepare for as part of their analytical development prior to finalization of the guidance. This will help them monitor and report on the right critical quality attributes (CQAs) of their CAR T products which is needed for characterization of the product’s safety and efficacy that is reported to health authorities.
1. Testing for previously administered CAR T in starting material. As CAR T therapies are currently being used in 2nd and 3rd line treatments, participants in clinical trials for new CAR T treatments may have previously administered CAR-T cells in their starting material (leukapheresis). The presence of CAR T cells other than the current treatment may have unexpected effects on cell manufacturing (e.g., expansion or transduction rates), potency, in vivo expansion, safety, or efficacy. For example, ongoing and future Chronic Lymphocytic Leukemia (CLL) clinical studies may include patients that have been previously treated with CD19-specific CAR T cells or other tumor antigen targeting CAR-T products. The persistence of previous CD19-specific CAR T cells in patients is not known, therefore an assumption is that some CD19-specific CAR T cells could still be circulating in the patient’s bloodstream. Those circulating CD19-specific CAR T cells could be collected in the leukapheresis and enter the manufacturing process for the new CAR-T product
Therefore, characterizing the patient’s starting material and cryopreserved drug product for the presence of CD19-specific CAR T cells is recommended. The analytical methods used to detect CD19-specific CAR T cells should be a matrix of molecular-based and flow cytometry-based methods. Results from these characterizations will be used in conjunction with patient outcomes to determine the safety risks from treating patients with varying amounts of CD19-specific CAR T cells in their starting material. If previously administered CAR-T products are detected, subsequent testing should include evaluation of the vector copy number (VCN) in the final product, both for the newly introduced and previously administered CAR T cells due to the risks associated with increased vector integration frequencies1.
Like the presence of previously administered CAR Ts, other residual cell impurities such as hematopoietic stem cells, residual tumor cells, and non-viable cells, should also be evaluated. Deep product understanding through an expanded panel of characterization methods that monitor many different cellular attributes on patient starting material and final drug product is critical for effective product understanding.
2. Establishing manufacturing process controls. Due to patient or donor variability, cellular starting material can represent a major source of lot-to-lot variability. It is therefore critical to fully develop a comprehensive control strategy f for critical process parameters, intermediates and final drug product. This includes monitoring in-process cell viability, cell number, cell phenotype, CAR expression. Results from in-process tests can be used to guide manufacturing decisions at critical manufacturing steps. Establishing a deep understanding of the CQAs and the ability of analytical methods to measure and monitor those CQAs is especially important. This becomes even more crucial as the inevitable process changes and improvements are made. Analytical methods must be developed to be able to demonstrate the impact of process changes.
3. Implementing robust analytical testing. Analytical testing of CAR T cells is necessary to assure product safety, identity, quality, purity, and strength of the investigational product. CAR T innovators should employ a risk-based approach to determine product CQAs and associated analytical target profile for each method. This is followed by thorough method development and phase-appropriate method validation and method-life cycle management. Three critical capabilities to consider includes:
- Flow cytometry – Flow cytometry core facility ensures that CAR-T product identity, purity and residual cellular impurity and previously administered CAR-T cell understanding is established. In addition to the presence of certain cell populations in the final product previously discussed, running robustness studies is key. This includes defining the maximum holding times for samples: before staining, between staining, and during acquisition. Maintaining assay controls e.g., single-stained compensation controls for calculating compensation values, Fluorescence Minus One (FMO) controls to determine fluorescence spread and gating boundaries for minor populations, and isotype controls to identify the nonspecific binding.
- Molecular biology – The use of advanced molecular analytics including NGS, digital PCR, long-read sequence analysis, and single-cell qPCR may help to mitigate the risk of transgene integration that impacts the expression of important cellular genes and increases the risk of tumorigenicity,. This enables the ability to conduct full molecular analysis to characterize transgene integration, off-target insertional mutagenesis, and vector copy number as a function of CAR expressing cells.
- Potency – Potency and cellular functional analysis tests are conducting utilizing a matrix approach with orthogonal methods that can include cell-based bioassay cytotoxicity assays transduction control measurements, activation assays, cytokine secretion assays, reporter assays, physiologically-relevant invitro models, real-time impedance-based analysis, and metabolomics to establish a comprehensive understanding of CAR-T potency.
As CAR T and other methods of gene editing continue to mature and improve patient lives, innovator companies will need to continue to invest in analytical development and testing capabilities to get their products to market quickly and safely. In future pieces, we will explore the technology foundations needed to collect, store, and ultimately run these tests
- Retroviral and lentiviral vectors have been broadly used in Chimeric Antigen Receptor (CAR) T-cell therapy clinical trials. These vectors have the capacity to integrate permanently into host cell DNA. There is an increased risk of oncogenesis if the vector copy number (VCN) per cell is high. The Food and Drug Administration (FDA) recommends that the VCN shall be <5 copies per genome. Accurate and rapid measurement of VCN is an important quality control step required for release of CAR T-cell products for patient infusion.
Center for Breakthrough Medicines (CBM) is an Advanced Therapy CDMO dedicated to addressing the challenges with bringing breakthrough therapies to patients. CBM offers pre-clinical through commercial manufacturing capabilities spanning process development, plasmid DNA, viral vector and cell therapy production, and a full suite of testing and analytical capabilities. Through a single-source, end-to-end solution, CBM accelerates time to market without compromising quality.
In need of immediate assistance with your cell therapy manufacturing? Contact us here or simply call to speak with a CBM expert: 866-274-4009.
